Have a Doctor’s Referral?Book now
Longer days and rising temperatures can only mean one thing: summer is right around the corner! At Kintec, we share your excitement to get outdoors and hit the trails.
However, we also recognize that hiking can come with its fair share of challenges and potential injuries. From blisters and sprains to tendonitis and plantar fasciitis, these common hiking injuries can put a damper on your adventure.
That’s why we are here to provide you with expert advice and practical solutions to keep you pain-free and moving forward. In this blog post, we will delve into common hiking injuries, exploring prevention strategies and effective treatment methods. So lace up your boots and get ready to equip yourself with the knowledge and tools you need to conquer the trails with confidence.
Sprained ankles rank as one of the most prevalent injuries encountered while hiking. Picture this: you’re hiking when suddenly your foot catches on a root, causing your ankle ligaments to stretch and tear in response to the abrupt twist or turn. Uneven terrain, loose rocks, tree roots, and slippery surfaces increase the likelihood of spraining an ankle while hiking.
Prevention
To prevent sprains, wear hiking shoes or boots that provide adequate ankle support such as the Hoka Kaha 2. Opt for footwear with sturdy construction and ankle cuffs that can help stabilize your ankles and reduce the risk of twisting or rolling.
Prior to hitting the trail, dedicate time to warm-up exercises that increase blood flow and loosen up your muscles. Focus on stretching your ankles, calves, and feet to enhance their flexibility and range of motion. This can help prepare your lower limbs for the demands of hiking and reduce the likelihood of sprains.
Treatment
If you do experience a sprain, stop hiking immediately. Rest, ice, compression, and elevation (RICE) are the standard treatment for sprains. Follow these steps:
If you are a seasoned hiker you may be all too familiar with painful blisters and how it can be difficult to continue hiking. Blisters occur when the skin rubs against shoes, socks, or other gear, causing friction. Often, heat or moisture can exacerbate the likelihood of a blister.
Prevention
To prevent blisters, make sure that your shoes fit well and that your socks are made of a moisture-wicking material. Synthetic or wool socks are ideal choices, as they effectively manage moisture. Cotton socks should be avoided due to their tendency to retain moisture and amplify the risk of blisters. If your feet do get wet during a creek crossing, be prepared with a fresh pair of dry socks. Additionally, prior to starting your hike consider applying moleskin or blister pads to areas that are prone to blisters.
Treatment:
It’s important to pay close attention to your feet while you hike. Early signs of a blister are called a ‘hot spot’. The area may be slightly red but if promptly identified and managed, it may not turn into a full-grown blister.
If you do develop a blister while hiking, stop and address it immediately. Clean the area with an antiseptic wipe. Consider covering the blister with moleskin or a blister pad to protect the area. If the blister is large or painful, consider taking a break from hiking or adjusting your shoes or socks to reduce friction.
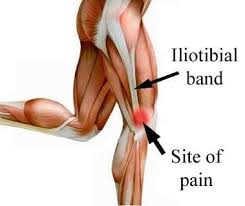 ITB Friction Syndrome is often found in hikers who embark on long-distance treks or repetitive downhill descents. The iliotibial band is a thick band of tissue that runs along the outside of the thigh, connecting the hip to the shinbone. When the ITB becomes irritated or inflamed due to excessive friction, it can lead to sharp pain and discomfort on the outer side of the knee. This pain typically intensifies during activity and can significantly impede a hiker’s progress.
ITB Friction Syndrome is often found in hikers who embark on long-distance treks or repetitive downhill descents. The iliotibial band is a thick band of tissue that runs along the outside of the thigh, connecting the hip to the shinbone. When the ITB becomes irritated or inflamed due to excessive friction, it can lead to sharp pain and discomfort on the outer side of the knee. This pain typically intensifies during activity and can significantly impede a hiker’s progress.
Prevention
Preventing ITB friction syndrome is important for hikers aiming to enjoy their adventures without the burden of knee pain. By following a few key strategies, hikers can reduce the risk of developing this condition:
Treatment
If symptoms occur, rest is essential to allow the inflamed ITB to heal. Hikers should temporarily avoid activities that aggravate the pain and provide ample time for recovery. Applying ice packs to the affected area can help reduce swelling and alleviate discomfort.
Engaging in targeted stretching exercises can help alleviate tightness in the ITB and surrounding muscles. Gentle stretches for the hip, thigh, and ITB, such as standing hip stretches and seated ITB stretches, can provide relief and promote flexibility. Additionally, foam rolling the ITB can help reduce tension and improve blood flow to the area, aiding in recovery.
Head to our ITBFS treatment guide to learn more.
Achilles tendinitis is another common injury that hikers may encounter during their adventures. It refers to the inflammation of the Achilles tendon, which is the thick cord of tissue that attaches calf muscles to the heel bones. Hikers often experience tendinitis in this area due to repetitive motions, overuse, improper form or technique, or inadequate rest and recovery.
Prevention
Proper hiking shoes can reduce the risk of Achilles tendinitis. Ensure you have appropriate footwear that provides adequate support and cushioning for your feet and ankles. Look for hiking shoes or boots with good arch support, cushioned soles, and a comfortable fit.
Avoid sudden increases in the intensity and duration of your hikes. Gradually build up your hiking routine, allowing your body, especially your Achilles tendon, to adapt and strengthen over time. This progressive approach helps prevent overuse and reduces the risk of Achilles tendinitis. Be mindful of your body’s signals and give yourself enough rest and recovery between hikes.
Finally, incorporate exercises that target the calf muscles and promote strength and flexibility. Strengthening exercises, such as calf raises and eccentric heel drops, can help improve the resilience of the Achilles tendon. Stretching exercises for the calf muscles, such as calf stretches and heel cord stretches, can enhance their flexibility and reduce strain on the tendon.
Treatment
If tendinitis symptoms occur, hikers should rest the affected area, apply ice to reduce inflammation, and consider using compression and elevation to alleviate pain and swelling. It’s important to seek medical advice for a proper diagnosis and to develop a treatment plan that may include physical therapy, pain management, and targeted exercises to promote healing and prevent further injury.
For more treatment tips view our complete guide here.
Plantar fasciitis causes pain and discomfort in the heel or arch of the foot. It occurs when the plantar fascia, a thick band of tissue that supports the arch, becomes inflamed or irritated. Hikers are at a higher risk of developing plantar fasciitis due to the repetitive impact and strain placed on the feet during long hikes or hikes on uneven terrain. Factors such as improper footwear, tight calf muscles, overpronation, or sudden increases in activity can contribute to the development of plantar fasciitis.
Prevention
To prevent plantar fasciitis we recommend:
Treatment
The key to quick recovery from plantar fasciitis is incorporating a combination of treatments including foot orthotics, proper footwear, foot rollers, as well as stretching, mobility, and strengthening exercises.
If symptoms arise, hikers should rest the affected foot and avoid activities that aggravate the pain. Modify your hiking routine to reduce stress on the plantar fascia and consider shorter hikes until the foot has had time to heal.
A rolling device is a simple and effective option that is convenient and easy to use for plantar fasciitis home treatment. It works by helping to stretch out the plantar fascia, which improves blood flow to the area, promoting healing and relieving pain.
Additionally, orthotics are clinically proven to reduce pain and improve function in patients with plantar fasciitis. Custom orthotics are insoles for your shoes that we manufacture in our lab specifically for you as part of your personalized treatment plan.
Custom orthotics work by providing support exactly where you need it based on your unique biomechanics and feet. They alleviate stress on the plantar fascia and also distribute the pressure of your body weight along the bottom of your entire foot.
Learn more about custom orthotics here.
View Kintec’s complete treatment guide here.
At Kintec, we are committed to helping you stay active on your feet for life. Our Canadian Certified Pedorthists will perform a thorough analysis of your feet, biomechanics, and history, and develop a comprehensive and personalized treatment plan for you.
Our goal with assessment and treatment is to:
If you have any questions, please call us at 604-200-3338 or make an appointment to visit us in-store.