Pregnancy, Foot Pain, and Biomechanical Strain: An Overlooked Maternal Health Gap
By: Kelly Robb PhD, C Ped (C)
Pregnancy is a transformative journey — but it also brings significant physical changes that often go underrecognized, especially when it comes to the feet. As the body adapts to support new life, it undergoes rapid hormonal, structural, and biomechanical changes. These adaptations often result in foot pain, joint instability, and altered movement patterns — all of which can compromise a pregnant woman’s comfort, mobility, and long-term musculoskeletal health. Yet one simple, evidence-based intervention remains widely underutilized: custom foot orthotics.
The Hidden Problem: Pregnancy Alters the Body from the Ground Up
Pregnancy-related foot discomfort isn’t just common — it’s predictable, based on the biomechanical demands placed on the body. Understanding these changes is key to preventing long-term strain and dysfunction:
-
Relaxin Loosens Ligaments
The hormone relaxin, released during pregnancy to prepare the pelvis for childbirth, affects not only the pelvic region but also ligaments throughout the entire body, including those in the feet and lower limbs. This systemic increase in ligamentous laxity can result in fallen arches, joint instability, and overpronation (excessive inward rolling of the foot), which may contribute to musculoskeletal pain in the feet, ankles, knees, or hips, and can impair postural stability. Studies indicate that up to 70% of pregnant individuals experience structural changes in the feet, including arch collapse and increased foot length, primarily due to increased ligamentous laxity and mechanical load.
-
Weight Gain and Postural Shifts
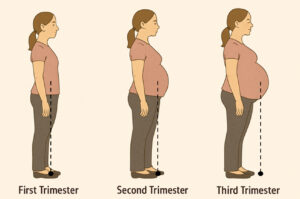
As pregnancy progresses, the growing baby and expanding uterus lead to a significant redistribution of body mass, shifting the center of gravity forward. This anterior shift places increased pressure on the feet — particularly the arches and forefoot — and can contribute to foot discomfort, flattening of the arches (overpronation), and even swelling due to fluid retention and vascular changes.
To maintain balance and stability in response to these changes, many pregnant women develop an altered gait or stance, often characterized by a wider base of support, increased lumbar lordosis (inward curvature of the lower spine), and changes in joint mechanics. These compensatory adaptations can place additional biomechanical strain on the knees, hips, and lower back. The increased production of relaxin, further exacerbates musculoskeletal instability, making the joints more susceptible to stress and misalignment.
As a result, many women experience common musculoskeletal complaints during pregnancy, including lower back pain, pelvic girdle pain, and joint discomfort, which are often interconnected with the body’s efforts to accommodate the shifting weight and maintain postural control.
-
Foot Swelling (Edema)
Swelling and discomfort from fluid retention—particularly in the feet and lower legs—are a common challenge for expectant mothers. In fact, nearly 75% of women experience this issue, most often during the third trimester. As blood volume increases and the growing uterus puts pressure on major veins, the return of blood from the lower body slows, causing fluid to accumulate. Maternity compression can be quite helpful to alleviate fatigue and edema (https://www.kintec.net/blog/compression-socks/), although fail to address the disruptions to normal foot function and the challenges in finding comfortable footwear that adapts to fluid fluctuations.
-
Changes in Foot Size and Gait
During pregnancy, many women experience an increase in shoe size, primarily due to foot widening and arch flattening. At the same time, gait adaptations commonly occur, including reduced stride length, increased step width, and slower walking speed. These changes are compensatory responses to the anterior shift in the center of mass and are aimed at enhancing stability. However, they can also lead to greater energy expenditure and may introduce new sources of fatigue and postural strain.
Current Foot Orthotics Overlook the Unique Needs of Pregnant and Postpartum Women
Despite the well-documented physical changes that occur during pregnancy, custom foot orthotics are rarely discussed or prescribed as part of prenatal care. This represents a missed opportunity, considering their demonstrated ability to:
- Support the arch and counteract ligament laxity;
- Stabilize foot joints and reduce excessive pronation;
- Improve gait mechanics and posture;
- Redistribute pressure to relieve pain; and
- Enhance balance and reduce fatigue during movement.
In non-pregnant populations, orthotics are a standard treatment for similar symptoms. Yet for pregnant women, recommendations often stop at advising supportive footwear—if the issue is acknowledged at all.
More critically, most commercial and custom orthotics are not designed to address the dynamic biomechanical changes that occur during and after pregnancy. Typically based on gait patterns observed in non-pregnant individuals, these devices often fail to accommodate:
- Progressive ligamentous laxity;
- Rapid weight gain;
- Joint instability; and
- Shifting center of gravity and evolving gait mechanics.
As a result, standard orthotics may prove ineffective, uncomfortable, or even harmful during pregnancy. Given the frequent changes in foot size (e.g., lengthening, widening) and fluctuating edema, how can fixed-template orthotics truly serve the maternal foot? There is a clear need for adjustable, adaptive orthotic solutions that evolve with the body throughout pregnancy.
Postpartum, the issue continues. Foot biomechanics often do not return to pre-pregnancy norms—especially after multiple pregnancies or cesarian deliveries. Yet orthotic prescriptions typically end at delivery, overlooking a critical period of recovery when women are physically active in caregiving roles but still experiencing pain or instability.
Once again, the potential benefits of orthotics are missed—both during and after pregnancy and may serve a valuable rehabilitative tool during postpartum recovery.
Time to Step Up: A New Standard for Prenatal Care
Pregnant women deserve more than generic advice to “rest and wear comfortable shoes.” Pregnant women also deserve tailored solutions to meet their evolving needs during pregnancy and postpartum. Foot health should be part of routine prenatal care — not an afterthought. As a woman’s body undergoes significant biomechanical changes during pregnancy and postpartum — including weight gain, ligament laxity, altered gait, and changes in foot structure — her footwear and orthotic support must evolve in tandem.
Custom-designed foot orthotics that adapt to these physiological shifts can help reduce pain, improve balance, and prevent long-term musculoskeletal issues. From trimester to recovery, orthotics should support not just the feet but the entire kinetic chain, responding to the changing demands placed on the body. Investing in dynamic, stage-specific orthotic solutions is an essential step toward comprehensive maternal health care.
Closing the Gap and Final Thoughts
Pregnancy challenges the body in extraordinary ways. By recognizing the biomechanical impact on foot health — and responding with targeted, non-invasive support — we can improve comfort, reduce unnecessary strain, and help women move through pregnancy with confidence and stability. It’s time to support pregnancy from the ground up.
To provide effective care, clinicians and foot orthotic manufacturers must recognize that pregnancy and postpartum represent a distinct clinical category. Current orthotic designs are often insufficient because they fail to accommodate the dynamic, evolving, and gender-specific biomechanical changes of pregnancy. There is an urgent need for pregnancy-specific orthotic solutions and a more inclusive, responsive approach to foot health in maternal care.
No Comments