The Complete Treatment Guide for Plantar Fasciitis
What Is Plantar Fasciitis?
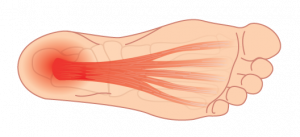
Plantar fasciitis (fash-ee-ahy-tis) is the most common cause of foot pain1. It’s usually described as sharp pain in the heel, especially when you take your first steps in the morning.
It occurs when there is a structural breakdown of your plantar fascia2, which is a thick fibrous band of tissue (fascia) on the bottom (plantar side) of our feet that connects your heel bone to your toes. This often leads to small tears in the tissue causing recurring cycles of inflammation and pain3.
When your plantar fascia become damaged and inflamed, the resulting pain can severely limit your ability to stay active on your feet.
Do You Have Plantar Fasciitis?
Symptoms of Plantar Fasciitis
Depending on your feet and activities, plantar fasciitis may cause sudden pain in your heel or appear gradually with the pain worsening over time.
If you’re suffering from some or all of the following symptoms, your heel pain is most likely caused by plantar fasciitis:
- “first-step” pain—sharp heel pain in the morning, and again when standing or walking after long periods of sitting
- pain eases initially with activity but returns in the afternoon or evening
- pain is worse at the base (and slightly inside/medial) of your heel
- pain increases with long periods of time spent on your feet
- pain may be intermittent and can last for months to years
What Causes Plantar Fasciitis?
Research indicates there is a combination of factors that lead to plantar fasciitis4.
It occurs when there is a structural breakdown of your plantar fascia5 — the tissue (fascia) on the bottom (plantar side) of our feet that connects your heel bone to your toe. This often leads to small tears in the tissue causing recurring cycles of inflammation and pain6.
Note: Structural changes in your plantar fascia can happen months or even years before you experience symptoms.
The following factors can increase your risk of developing plantar fasciitis7:
INTERNAL FACTORS
- abnormalities in your plantar fascia, such as: increases in nerve endings; thickening; altered tissue composition; and small tears;
- limited ability to flex your ankle joint up and down can create more tension on the heel bone;
- tight muscles in your calves, hamstrings or Achilles tendon can create more tension on the heel bone8;
- low arches and high arches increase stress on plantar fascia with foot strike9;
- overpronation (if your foot rolls excessively down and inward when you walk);
- degeneration in the fat pad of the heel (associated with aging);
- age and gender: most common in women aged 40 – 60 years;
- obesity: excess weight adds stress and strain on the plantar fascia
EXTERNAL FACTORS
- work and occupations that require standing or walking on hard surfaces for long periods of time;
- sports and activities that cause overuse and added stress on the plantar fascia, such as running, soccer, dancing; any sports requiring fast increase in the distance, intensity, duration or repetitive impact of weight on the feet
- shoes that strain your plantar fascia, such as high heels; shoes without any arch and heel support; and older, worn-out shoes.
How Do We Assess Your Plantar Fasciitis?
When you book an appointment with one of our Canadian Certified Pedorthists, we’ll perform a detailed assessment, which includes:
- a physical examination your feet
- a video gait analysis to evaluate the biomechanics of your feet and lower limbs—we analyze your pattern of movement when walking and determine how your feet and legs work together to produce movement
- a review of your activities, symptoms, and history of your foot and heel pain
- a personalized treatment plan for your unique situation
Our One2One program will provide you with the highest level of safety and personalized service for your assessments, as well as your orthotic, footwear and bracing needs.
How to Treat Plantar Fasciitis
Your goals for treatment are to: ✓ reduce inflammation and pain ✓ heal your tissues ✓ get you active on your feet again ✓ prevent re-injury
Most people respond well to treatment and recover within 6 to 8 weeks (although it can vary depending on the underlying cause, history, and severity of your condition).
Tip: The sooner you begin treatment, the better. Ignoring your plantar fasciitis may result in chronic heel pain that continues to limit your ability to stay active on your feet. Without treatment, you may find yourself changing the way you walk to minimize the pain, which can lead to further foot, knee, hip or back problems.
As part of your assessment with one of our Canadian Certified Pedorthists, we’ll provide a personalized treatment plan that may include some or all of the following treatments:
1. Rest
Rest is extremely important to healing. Use pain as your guide: if your feet hurt while standing or walking, take as many breaks as possible and limit the time spent on your feet.
2. Ice
- Ice the area under the heel and arch several times a day—especially after prolonged standing, walking and activity—to reduce inflammation and promote healing.
- A frozen water bottle is a great way to relieve pain after activity or a long day on your feet.
- Gel icepacks can also be used by wrapping them around your foot with tensor bandage for about 5-10 minutes (remember to always protect your skin with a layer of clothing or dish towel to prevent an ice burn).
3. Plantar Fasciitis Massage
A rolling device is a simple and effective option that is convenient and easy to use for plantar fasciitis home treatment. It works by helping to stretch out the plantar fascia, which improves blood flow to the area, promoting healing and relieving pain.

4. Plantar Fasciitis Exercises

Calf Stretch (Gastrocnemius and Soleus)
- step one foot forward, elevating the forefoot and keeping the heel on the ground
- bend the front knee approximately 15 to 20 degrees
- switch to the other leg and repeat
- complete 3 sets of 30 seconds each

Forefoot Extension Stretch
- stand shoulder-width apart and place one foot ahead of the other
- contract the calf muscle of the back leg to lift the heel
- raise the heel until you have lifted onto the forefoot
- complete 5 sets of 15 repetitions each
We recommend 3 additional stretches in our plantar fasciitis exercises PDF: Download our FREE Guide to Plantar Fasciitis Recovery
5. Orthotics for Plantar Fasciitis
Orthotics are clinically proven11 to reduce pain and improve function in patients with plantar fasciitis.
Custom orthotics are insoles for your shoes that we manufacture in our lab specifically for you as part of your personalized treatment plan.
Custom orthotics work by providing support exactly where you need it based on your unique biomechanics and feet. They alleviate stress on the plantar fascia, and also distribute the pressure of your bodyweight along the bottom of your entire foot.
Learn more about custom orthotics.

We also offer the best over-the-counter insoles that can help heal and prevent plantar fasciits. Visit a Kintec store today and our Fit Experts will help you find the perfect fit.
6. Best Shoes for Plantar Fasciitis
The right shoes reduce strain on your plantar fascia, which alleviates pain, promotes healing, and helps prevent future injury.
Footwear Tips:
- For a flexible foot, choose a structured shoe with torsional stability and a stiff heel counter.
- For a foot that is not flexible, choose a shoe with good shock absorption to reduce impact to the plantar fascia.
- Choose a stiff front rocker to help propel your foot forward and reduce stress on the plantar fascia.
- Avoid going barefoot and wear supportive shoes around the house. Choose slippers, sandals and flip flops with built-in arch support and heel cups.
We offer running shoes, casual shoes, and sandals to help heal and prevent plantar fasciitis. Visit a Kintec store today and our Fit Experts will help you find the perfect fit from our line of hand-selected footwear.
7. Modify Your Activities and Exercise
When you’re suffering from plantar fasciitis, we recommend switching to lower impact exercises, such as cycling and swimming, so you can stay active and allow your plantar fascia to heal.
8. Anti-Inflammatory Cream
Over-the-counter anti-inflammatory cream can be an effective way to reduce inflammation and pain. We offer a cream with all-natural active ingredients such as calendula oil, eucalyptus oil, and peppermint oil that can applied with gentle massage to your arch and heel to relieve your symptoms.

9. Night Splints
A night splint holds your calf and plantar fascia in an optimal position for healing. When the tissues are in a stable, elongated position, there is less tension allowing the plantar fascia to heal and recover.
Night splints can be very helpful if you: have tried other methods; have very painful and stubborn plantar fasciitis; and experience stabbing pain when you take your first steps in the morning.

How to Prevent Plantar Fasciitis
We recommend ongoing activities and care of your feet includng:
✓ daily stretches and massage to improve strength, flexibility and circulation
✓ appropriate and supportive footwear for all of your activities (work, travel, sport)
✓ custom orthotics to correct and/or support your unique feet and biomechanics
✓ monitoring and adjusting the frequency of high impact activities, and time spent on your feet, to help minimize stress on the plantar fascia
Do you have stubborn plantar fasciitis?
Structural breakdown of your plantar fascia can happen months or even years before you experience painful symptoms.
These changes can also affect the healthy blood supply to the tissues, making it even harder for the cells to repair12. As a result, plantar fasciitis can be very stubborn and take longer to heal in some patients.
Although research indicates that with early diagnosis and timely treatments, 80% of patients’ symptoms resolve within the first year, 20% of patients will experience persistent symptoms13.
If you’re one of the 20% suffering from recurring and stubborn plantar fasciitis, we can help.
Book an assessment today
Our Canadian Certified Pedorthists will perform a thorough analysis of your feet, biomechanics and history, and develop a comprehensive and personalized treatment plan for you.
Our One2One program will provide you with the highest level of safety and personalized service for your assessments, and all of your orthotic, footwear and bracing needs.
Our goal with assessment and treatment is to:
- provide you with education, support, and a personalized treatment plan
- minimize your risk of recurrent plantar fasciitis
- help you stay active on your feet, for life
If you have any questions, please call us at 604-200-3338 or make an appointment to visit us in-store.

1 Riddle, Daniel & M Schappert, Susan. (2004). Volume of Ambulatory Care Visits and Patterns of Care for Patients Diagnosed with Plantar Fasciitis: A National Study of Medical Doctors. Foot & ankle international / American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society. 25. 303-10. 10.1177/107110070402500505.
2 Ryan MB, Wong AD, Gillies JH, et alSonographically guided intratendinous injections of hyperosmolar dextrose/lidocaine: a pilot study for the treatment of chronic plantar fasciitis British Journal of Sports Medicine 2009;43:303-306.
3 Lemont H, Ammirati KM, Usen N. (2003). Plantar fasciitis: a degenerative process (fasciosis) without inflammation. Journal of American Podiatric Medical Association. May-Jun;93(3):234-7.
4 Gutteck, N., Schilde, S., & Delank, K. S. (2019). Pain on the Plantar Surface of the Foot. Deutsches Arzteblatt international, 116(6), 83–88. doi:10.3238/arztebl.2019.0083
5 Lemont H, Ammirati KM, Usen N. (2003). Plantar fasciitis: a degenerative process (fasciosis) without inflammation. Journal of American Podiatric Medical Association. May-Jun;93(3):234-7.
6 Lemont H, Ammirati KM, Usen N. (2003). Plantar fasciitis: a degenerative process (fasciosis) without inflammation. Journal of American Podiatric Medical Association. May-Jun;93(3):234-7.
7 Schwartz, E. N., & Su, J. (2014). Plantar fasciitis: a concise review. The Permanente journal, 18(1), e105–e107. doi:10.7812/TPP/13-113
8 Bolívar YA, Munuera PV, Padillo JP.(2013) Relationship between tightness of the posterior muscles of the lower limb and plantar fasciitis. Foot Ankle Int. 2013 Jan;34(1):42-8. doi: 10.1177/1071100712459173.
9 Reid DC. Running: injury patterns and prevention. Sports Injury Assessment and Rehabilitation. New York, NY: Churchill Livingstone; 1992. 1131-58.
10 Ryan M, Hartwell J, Fraser S, Newsham-West R, Taunton J. (2014). Comparison of a physiotherapy program versus dexamethasone injections for plantar fasciopathy in prolonged standing workers: a randomized clinical trial. Clin J Sport Med. 2014 May;24(3):211-7. 10.1097/JSM.0000000000000021.
11 Michael T. Gross, PT, PhD James M. Byers, MPT, Jeffrey L. Krafft, MPT, Eric J. Lackey, MPT, Kathy M. Melton, MPT. (2002). The Impact of Custom Semirigid Foot Orthotics on Pain and Disability for Individuals With Plantar Fasciitis. Journal of Orthopaedic & Sports Physical Therapy. Volume 32, Number 4, p
12 Miller, L. E., & Latt, D. L. (2015). Chronic Plantar Fasciitis is Mediated by Local Hemodynamics: Implications for Emerging Therapies. North American journal of medical sciences, 7(1), 1–5. doi:10.4103/1947-2714.150080
13 Miller, L. E., & Latt, D. L. (2015). Chronic Plantar Fasciitis is Mediated by Local Hemodynamics: Implications for Emerging Therapies. North American journal of medical sciences, 7(1), 1–5. doi:10.4103/1947-2714.150080


